In Italy, only 20 out of 65,000 chronic Lupus patients got COVID-19.
In an article published in Il Tempo, one of Italy’s leading independent newspapers (Britannica.com), Annalisa Chiusolo, a prominent pharmacology researcher, described the mechanism of action of SARS-CoV-2. By understanding this mechanism, it is possible to target and select the most effective drugs against COVID-19 with accuracy and precision. The coronavirus affects the ability of the hemoglobin to transport oxygen, creating the preconditions for lung complications, known to be associated with COVID-19: breathlessness, acute respiratory distress syndrome, and death.
Discovering the theory of viral replication is the first step of any verification. Science proceeds by refutation or confirmation. If this thesis were confirmed, many unknowns would be explained. For example, why COVID-19 affects more men, people with diabetes, fewer women in general, and even fewer pregnant women, very few children, and people with thalassemia. It would close the circle.

But let's get down to the theory.
The virus needs porphyrins for its survival (probably for its replication), so it attacks the hemoglobin (the protein that carries oxygen in the blood), in particular, the OFR10 and OFR3 proteins attack the beta chain, and orph1ab subtracts the porphyrin. The concepts seem a bit abstruse for a layman, but simply speaking, this translates into less oxygen available to the body, with consequent accumulation of carbon dioxide. Thus, the lung cells enter into a state of distress and become the site of the cytokine storm – that is, an enormous immune response – responsible for the acute inflammation that characterizes COVID-19 pneumonia.
The value of hemoglobin in the blood can be an important parameter to assess the SARS- CoV-2 infection: in men, the average value of Hb (hemoglobin) is higher than in women. This would explain the higher incidence of COVID-19 pneumonia in men compared to women, the lower incidence, and the better prognosis in children and pregnant women, where Hb values are lower due to an increased need for iron, which makes less available the "nutrition" of the virus. In elderly or middle-aged patients with diabetes, pneumonia from COVID-19 has a higher incidence, therefore linked to increased Hb glycated in the blood, and therefore there is more "nourishment" for the virus.
The viral damage, therefore, is systemic, i.e., it affects the blood and is not confined to the lung alone. This would also explain the birth of healthy babies from COVID-19 positive mothers. Because in fetal Hb – stay with me, we will now use some technical concepts – two gamma chains replace the two beta chains, a difference is the presence of a residual serine, instead of a histidine present in the same position of the beta chain, probably responsible for the binding with viral proteins, which could mimic the action of 2,3bifosfoglycerate.
Now, let's go back to using more understandable language.
All this would explain the lower incidence and better course of the disease in infants, missing the main site of action of viral proteins, i.e., the beta chains of Hb. In short, in infants, the same concept of "nutrition" for the coronavirus is missing.
The same goes for a chronic pathology called Beta-thalassemia, where the "beta" chains of hemoglobin (the target of the virus) are deficient or even absent. This would demonstrate the lower incidence and better prognosis and course of the pathology in thalassaemic beta-thalassaemias, which in Italy are widespread in Mediterranean areas such as Puglia, Sicily, and Sardinia (particularly in the south) where there is a thalassaemia rate of 12% (alpha and beta). To confirm this theory, there is a scientific publication that has put in relation the subjects affected by beta-thalassaemia and COVID-19, in the data taken from PubMed: as of April 10, 2020, 11 cases of COVID-19 positive beta talassaemia were recorded in Northern Italy, where the rate of contagiousness is higher. Ten of them are affected by thalassaemia dependent on transfusion, the most severe form, only one by thalassaemia is not reliant on transfusion.
However, all patients who contracted the virus had comorbidities, very serious diseases: splenectomized, pulmonary hypertension, lymphoma, and chemotherapy. Despite this multi-pathological picture, there were no deaths, no cytokine storms, or severe SARS in the 11 subjects.
Earlier, Dr. Zelenko shared his detailed coronavirus treatment plan based on his own experience in treating COVID-19 patients.

Once the main mechanism of action of the virus has been revealed, many other things can be understood.
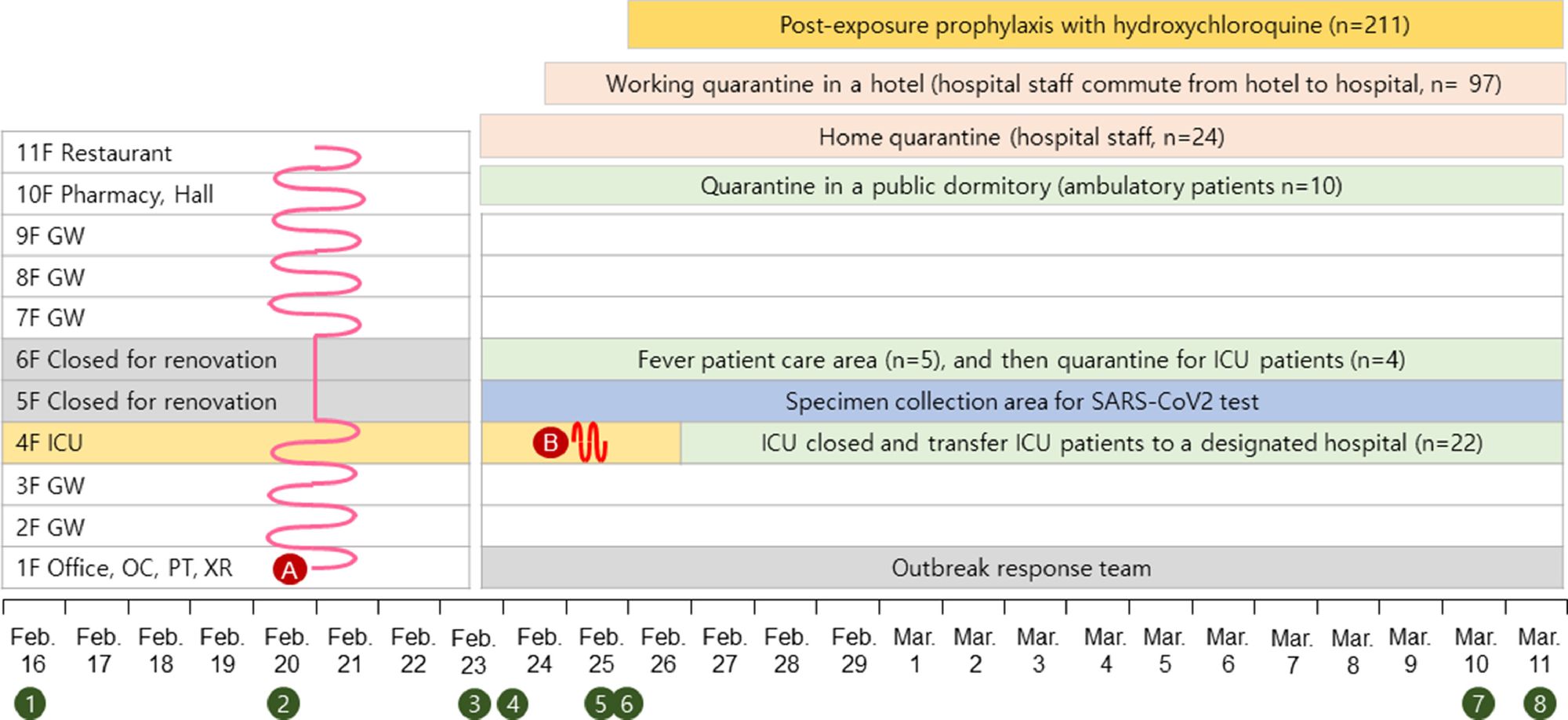
For example, the central mechanism of action of hydroxychloroquine, and its effectiveness in combating COVID-19, can now be fully explained and understood. What this mechanism consists of is immediately stated: the drug, by binding itself permanently with ferriprotoporphyrin (of the Hb group Eme), removes the substrate from the viral proteins and also becomes an important means of prophylaxis. Although there are still no Italian publications on the effectiveness of hydroxychloroquine as a "shield" from the virus, among the directors of infectious disease departments, specialists, primary care physicians, and general practitioners contacted during this research, many have admitted – under the subheading – to using the drug as a “prophylaxis”, i.e., to prevent contagion.
Healthcare professionals who are in close contact with infectious patients take the drug in advance, precisely to decrease the likelihood of infection. For now, there is a recent publication, involving 211 people, to support this ”prophylactic” effect. It was published in the International Journal of Antimicrobial Agents, the official organ of the International Society of Antimicrobial Chemotherapy. Of 211 people exposed to COVID-19 positive individuals and prophylaxis with hydroxychloroquine, none were infected.

Finally, further confirmation of this hypothesis is provided by the data collected in the register of the SIR (Italian Society of Rheumatology). In order to evaluate the possible correlations between chronic patients and COVID-19 SIR interviewed 1,200 rheumatologists throughout Italy to collect statistics on contagions. Out of an audience of 65,000 chronic patients (Lupus and Rheumatoid Arthritis), who systematically take Plaquenil/hydroxychloroquine, only 20 patients tested positive for the virus. Nobody died, and nobody is in intensive care, according to the data collected so far.